 Dust, cats, peanuts, cockroaches. An odd grouping, but one with a common thread: allergies — a major cause of illness in the United States. Up to 50 million Americans, including millions of kids, have some type of allergy. In fact, allergies account for the loss of an estimated 2 million schooldays per year.
Dust, cats, peanuts, cockroaches. An odd grouping, but one with a common thread: allergies — a major cause of illness in the United States. Up to 50 million Americans, including millions of kids, have some type of allergy. In fact, allergies account for the loss of an estimated 2 million schooldays per year.About Allergies
 An allergy is an overreaction of the immune system to a substance that's harmless to most people. But in someone with an allergy, the body's immune system treats the substance (called an allergen) as an invader and reacts inappropriately, resulting in symptoms that can be anywhere from annoying to possibly harmful to the person.
An allergy is an overreaction of the immune system to a substance that's harmless to most people. But in someone with an allergy, the body's immune system treats the substance (called an allergen) as an invader and reacts inappropriately, resulting in symptoms that can be anywhere from annoying to possibly harmful to the person.In an attempt to protect the body, the immune system of the allergic person produces antibodies called immunoglobulin E (IgE). Those antibodies then cause mast cells and basophils (allergy cells in the body) to release chemicals, including histamine, into the bloodstream to defend against the allergen "invader."
It's the release of these chemicals that causes allergic reactions, affecting a person's eyes, nose, throat, lungs, skin, or gastrointestinal tract as the body attempts to rid itself of the invading allergen. Future exposure to that same allergen (things like nuts or pollen that you can be allergic to) will trigger this allergic response again. This means every time the person eats that particular food or is exposed to that particular allergen, he or she will have an allergic reaction.
Who Gets Allergies?
The tendency to develop allergies is often hereditary, which means it can be passed down through your genes. However, just because you, your partner, or one of your children might have allergies doesn't mean that all of your kids will definitely get them, too. And someone usually doesn't inherit a particular allergy, just the likelihood of having allergies.
But a few kids have allergies even if no family member is allergic. A child who is allergic to one substance is likely to be allergic to others as well
Common Airborne Allergens
Some of the most common things people are allergic to are airborne (carried through the air):
•Dust mites are one of the most common causes of allergies. These microscopic insects live all around us and feed on the millions of dead skin cells that fall off our bodies every day. Dust mites are the main allergic component of house dust, which is made up of many particles and can contain things such as fabric fibers and bacteria, as well as microscopic animal allergens. Dust mites are present year-round in most parts of the United States (although they don't live at high altitudes), and live in bedding, upholstery, and carpets.
•Pollen is another major cause of allergies (most people know pollen allergy as hay fever or rose fever). Trees, weeds, and grasses release these tiny particles into the air to fertilize other plants. Pollen allergies are seasonal, and the type of pollen a child is allergic to determines when symptoms will occur. For example, in the mid-Atlantic states, tree pollination begins in February and lasts through May, grass from May through June, and ragweed from August through October; so people with these allergies are likely to experience increased symptoms during those times.
Pollen counts measure how much pollen is in the air and can help people with allergies determine how bad their symptoms might be on any given day. Pollen counts are usually higher in the morning and on warm, dry, breezy days, whereas they're lowest when it's chilly and wet. Although not always exact, the local weather report's pollen count can be helpful when planning outside activities.
•Molds, another common allergen, are fungi that thrive both indoors and out in warm, moist environments. Outdoors, molds may be found in poor drainage areas, such as in piles of rotting leaves or compost piles. Indoors, molds thrive in dark, poorly ventilated places such as bathrooms and damp basements, and in clothes hampers or under kitchen sinks. A musty odor suggests mold growth. Although molds tend to be seasonal, many can grow year-round, especially those indoors.
•Pet allergens from warm-blooded animals can cause problems for kids and parents alike. When the animal — often a household pet — licks itself, the saliva gets on its fur or feathers. As the saliva dries, protein particles become airborne and work their way into fabrics in the home. Cats are the worst offenders because the protein from their saliva is extremely tiny and they tend to lick themselves more than other animals as part of grooming. Pet allergens are also present in dander, hair, and urine.
•Cockroaches are also a major household allergen, especially in inner cities. Exposure to cockroach-infested buildings may be a major cause of the high rates of asthma in inner-city kids
Common Food Allergens
The American Academy of Allergy, Asthma, and Immunology estimates that up to 2 million, or 8%, of kids in the United States are affected by food allergies, and that eight foods account for most of those food allergy reactions in kids: eggs, fish, milk, peanuts, shellfish, soy, tree nuts, and wheat.
•Cow's milk (or cow's milk protein). Between 1% and 7.5% of infants are allergic to the proteins found in cow's milk and cow's milk-based formulas. About 80% of formulas on the market are cow's milk-based. Cow's milk protein allergy (also called formula protein allergy) means that the infant (or child or adult) has an abnormal immune system reaction to proteins found in the cow's milk used to make standard baby formulas, cheeses, and other milk products. Milk proteins can also be a hidden ingredient in many prepared foods.
•Eggs. One of the most common food allergies in infants and young children, egg allergy can pose many challenges for parents. Because eggs are used in many of the foods kids eat — and in many cases they're "hidden" ingredients — an egg allergy is hard to diagnose. An egg allergy usually begins when kids are very young, but most outgrow the allergy by age 5. Most kids with an egg allergy are allergic to the proteins in egg whites, but some can't tolerate proteins in the yolk.
•Seafood and shellfish. The proteins in seafood can cause a number of different types of allergic reactions. Seafood allergy is one of the more common adult food allergies and one that you don't always grow out of.
•Peanuts and tree nuts. Peanuts are one of the most severe food allergens, often causing life-threatening reactions. About 1.5 million people in the United States are allergic to peanuts. (Peanuts are not a true nut, but a legume — in the same family as peas and lentils, although people with peanut allergy don’t usually have cross-reactions to other legumes). Half of those allergic to peanuts are also allergic to tree nuts, such as almonds, walnuts, pecans, cashews, and often sunflower and sesame seeds. Like seafood allergy, peanut allergy is one you don't always grow out of.
•Soy. Like peanuts, soybeans are legumes. Soy allergy is more prevalent among babies than older children; about 30% to 40% of infants who are allergic to cow's milk are also allergic to the protein in soy formulas. Soy proteins, such as soya, are often a hidden ingredient in prepared foods.
•Wheat. Wheat proteins are found in many of the foods we eat — some are more obvious than others. As with any allergy, an allergy to wheat can happen in different ways and to different degrees. Although wheat allergy is often confused with celiac disease, there is a difference. Celiac disease is caused by a sensitivity to gluten, which is found in wheat, oat, rye, and barley. It typically develops between 6 months and 2 years of age and the sensitivity causes damage to the small intestine in a different way to the usual allergic reaction
Other Common Allergens
•Insect stings. For most kids, being stung by an insect means swelling, redness, and itching at the site of the bite. But for those with insect venom allergy, an insect bite can cause more severe symptoms. Although some doctors and parents have believed that most kids eventually outgrow insect venom allergy, a recent study found that insect venom allergies often persist into adulthood. An allergy evaluation is needed if wheezing and other signs of anaphylaxis are present after an insect sting or bite.
•Medicines. Antibiotics — medications used to treat infections — are the most common types of medicines that cause allergic reactions. Many other medicines, including over-the-counter medications, can also cause allergic reactions. If you suspect a medicine allergy, talk to your doctor first before assuming a reaction is a sign of allergy.
•Chemicals. Some cosmetics or laundry detergents can cause people to break out in an itchy rash. Usually, this is because someone has a reaction to the chemicals in these products. Dyes, household cleaners, and pesticides used on lawns or plants can also cause allergic reactions in some people.
Some kids also have what are called cross-reactions. For example, kids who are allergic to birch pollen might have reactions when they eat an apple because that apple is made up of a protein similar to one in the pollen. Another example is that kids who are allergic to latex (as in gloves or certain types of hospital equipment) are more likely to be allergic to kiwifruit, water chestnuts, or bananas
Signs and Symptoms
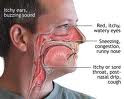
The type and severity of allergy symptoms vary from allergy to allergy and child to child. Allergies may show up as itchy eyes or an itchy nose, sneezing, nasal congestion, throat tightness, trouble breathing, and even shock (faintness or passing out).
Symptoms can range from minor or major seasonal annoyances (for example, from pollen or certain molds) to year-round problems (from allergens like dust mites or food). Allergies to dust mites are common to the eastern parts of the United States, but not in areas of high-altitude and low humidity (for example, like Colorado).
Because different allergens are more prevalent in different parts of the country and the world, allergy symptoms can also vary, depending on where you live. For example, peanut allergy is unknown in Scandinavia, where they don't eat peanuts, but is common in the United States, where peanuts are not only a popular food, but are also found in many of the things we eat.
Airborne Allergy Symptoms
Airborne allergens can cause something known as allergic rhinitis, which occurs in about 15% to 20% of Americans. It develops by 10 years of age and reaches its peak in the early twenties, with symptoms often disappearing between the ages of 40 and 60.
Symptoms can include:
•sneezing
•itchy nose and/or throat
•nasal congestion
•coughing
These symptoms are often accompanied by itchy, watery, and/or red eyes, which is called allergic conjunctivitis. (When dark circles are present around the eyes, they're called allergic "shiners.") Those who react to airborne allergens usually have allergic rhinitis and/or allergic conjunctivitis. If a person has wheezing and shortness of breath, the allergy may have progressed to become asthma.
Food Allergy Symptoms
The severity of food allergy symptoms and when they develop depends on:
•how much of the food is eaten
•the person's sensitivity to the food
Symptoms of food allergies can include:
•itchy mouth and throat when food is swallowed (some kids have only this symptom — called "oral allergy syndrome")
•hives (raised, red, itchy bumps)
•eczematous rash
•runny, itchy nose
•abdominal cramps accompanied by nausea and vomiting or diarrhea (as the body attempts to flush out the food allergen)
•difficulty breathing
•shock
Insect Venom Allergy Symptoms
Being stung by an insect that a child is allergic to may cause some of these symptoms:
•throat swelling
•hives over the entire body
•difficulty breathing
•nausea
•diarrhea
•shock
About Anaphylaxis
In rare instances, if the sensitivity to an allergen is extreme, a child may experience anaphylaxis (or anaphylactic shock) — a sudden, severe allergic reaction involving various systems in the body (such as the skin, respiratory tract, gastrointestinal tract, and cardiovascular system).
Severe symptoms or reactions to any allergen, from certain foods to insect bites, require immediate medical attention and can include:
•difficulty breathing
•swelling (particularly of the face, throat, lips, and tongue in cases of food allergies)
•rapid drop in blood pressure
•dizziness
•unconsciousness
•hives
•tightness of the throat
•hoarse voice
•lightheadedness
Anaphylaxis can happen just seconds after being exposed to a triggering substance or can be delayed for up to 2 hours if the reaction is from a food. It can involve various areas of the body.
Fortunately, though, severe or life-threatening allergies occur in only a small group of kids. In fact, the annual incidence of anaphylactic reactions is small — about 30 per 100,000 people — although those with asthma, eczema, or hay fever are at greater risk of experiencing them. Most anaphylactic reactions — up to 80% — are caused by peanuts or tree nuts
Diagnosing Allergies
Some allergies are fairly easy to identify because the pattern of symptoms following exposure to certain allergens can be hard to miss. But other allergies are less obvious because they can masquerade as other conditions.
If your child has cold-like symptoms lasting longer than a week or two or develops a "cold" at the same time every year, consult your doctor, who will likely ask questions about the symptoms and when they appear. Based on the answers to these questions and a physical exam, the doctor may be able to make a diagnosis and prescribe medications or may refer you to an allergist for allergy skin tests and more extensive therapy.
To determine the cause of an allergy, allergists usually perform skin tests for the most common environmental and food allergens. These tests can be done in infants, but they're more reliable in kids over 2 years old.
A skin test can work in one of two ways:
1.A drop of a purified liquid form of the allergen is dropped onto the skin and the area is pricked with a small pricking device.
2.A small amount of allergen is injected just under the skin. This test stings a little but isn't extremely painful. After about 15 minutes, if a lump surrounded by a reddish area appears (like a mosquito bite) at the injection site, the test is positive.
If reactions to a food or other allergen are severe, a blood test may be used to diagnose the allergy so as to avoid exposure to the offending allergen. Skin tests are less expensive and more sensitive than blood tests for allergies. But blood tests may be required in children with skin conditions or those who are extremely sensitive to a particular allergen.
Even if a skin test and/or a blood test shows an allergy, a child must also have symptoms to be definitively diagnosed with an allergy. For example, a toddler who has a positive test for dust mites and sneezes frequently while playing on the floor would be considered allergic to dust mites
Treating Allergies
There is no real cure for allergies, but it is possible to relieve symptoms. The only real way to cope with them is to reduce or eliminate exposure to allergens. That means that parents must educate their kids early and often, not only about the allergy itself, but also about what reaction they will have if they consume or come into contact with the allergen.
Informing any and all caregivers (childcare personnel, teachers, extended family members, parents of your child's friends, etc.) about your child's allergy is equally important.
If reducing exposure isn't possible or is ineffective, medications may be prescribed, including antihistamines (which you can also buy over the counter) and inhaled or nasal spray steroids.
In some cases, an allergist may recommend immunotherapy (allergy shots) to help desensitize your child. However, allergy shots are only helpful for allergens such as dust, mold, pollens, animals, and insect stings. They're not used for food allergies, and someone with food allergies must avoid that food.
Here are some things that can help kids avoid airborne allergens:
•Keep family pets out of certain rooms, like your child's bedroom, and bathe them if necessary.
•Remove carpets or rugs from your child's room (hard floor surfaces don't collect dust as much as carpets do).
•Don't hang heavy drapes and get rid of other items that allow dust to accumulate.
•Clean frequently.
•Use special covers to seal pillows and mattresses if your child is allergic to dust mites.
•For kids allergic to pollen, keep the windows closed when the pollen season is at its peak, change their clothing after they've been outdoors, and don't let them mow the lawn.
•Keep kids who are allergic to mold away from damp areas, such as basements, and keep bathrooms and other mold-prone areas clean and dry
Injectable Epinephrine
Food allergies usually aren't lifelong (although those to peanuts, tree nuts, and seafood can be). Avoiding the food is the only way to avoid symptoms while the sensitivity persists.
Doctors often recommend that caregivers of kids who are extremely sensitive to a particular food, have asthma in addition to the food allergy, or are allergic to insect venom carry injectable epinephrine (adrenaline) to counteract any allergic reactions.
Available in an easy-to-carry container that looks like a pen, injectable epinephrine is carried by millions of parents (and older kids) everywhere they go. With one injection into the thigh, the device administers epinephrine to ease the allergic reaction.
An injectable epinephrine prescription usually includes two auto-injectors and a "trainer" that contains no needle or epinephrine, but allows you and your child (if he or she is old enough) to practice using the device. It's vital that you familiarize yourself with the procedure by practicing with the trainer. Your doctor also can provide instructions on how to use and store injectable epinephrine.
Make sure kids 12 years or older keep injectable epinephrine readily available at all times. If your child is younger than 12, talk to the school nurse, teachers, and your childcare provider about keeping injectable epinephrine on hand in case of an emergency.
It's also important to ensure that injectable epinephrine devices are available in your home and in the homes of friends and family members if your child spends time there. Your doctor may also encourage your child to wear a medical alert bracelet. It's also wise to carry an over-the-counter antihistamine, which can help alleviate allergy symptoms in some people. But antihistamines should not be used as a replacement for the epinephrine pen.
Kids who have had to take injectable epinephrine should go immediately to a medical facility or hospital emergency department, where additional treatment can be given if needed. Up to one third of anaphylactic reactions can have a second wave of symptoms several hours following the initial attack, so these kids might need to be observed in a clinic or hospital for 4 to 8 hours following the reaction even though they seem well.
The good news is that only a very small group of kids will experience severe or life-threatening allergies. With proper diagnosis, preventive measures, and treatment, most kids can keep their allergies in check and live happy, healthy lives





No comments:
Post a Comment